As the start of the 2020-21 school year rapidly approaches, many of you have asked how I think schools should re-open. As a pediatrician who has cared for patients with COVID-19, a parent of 2 school-age children, and a mother of 2 children who had COVID-19 (1 of whom was hospitalized and had all the signs of possibly heading toward MIS-C), I have a unique perspective that I want to share. Know that this is my opinion, based on the limited yet emerging data we have about COVID-19 in kids, my personal and clinical experiences as a mother and pediatrician, and the reality we’re living in – which at the moment includes a surge in COVID-19 cases in most states, and a continued lack of adequate testing capacity for symptomatic and exposed individuals.
So how should schools re-open?
The reality is:
I don’t really know … nobody really knows!
The reality is:
The world has never seen a pandemic like this before. Re-opening schools is one of the biggest social and medical experiments our kids will ever face – except they don’t get to provide consent.
The reality is:
In this time of uncertainty, the only certain thing is that within the first week or two of starting school, there WILL be a child with a fever, headache, runny nose, cough, sore throat, stomach ache, vomiting, diarrhea (all possible symptoms of COVID-19).
What Happens After a Child is Exposed to COVID-19 in School?
When there is a child in class with possible COVID-19, there are no clear guidelines what his/her classmates and educators should do – who should get tested and how long after exposure, is quarantine necessary and for how long, should the class quarantine together as a cohort?
The CDC defines an “exposure” as an “individual who has had close contact (< 6 feet) for ≥ 15 minutes” to a person with COVID-19 that is laboratory-confirmed or has a “clinically compatible illness,” whether or not they test positive. The CDC considers “exposure to have occurred “irrespective of whether the person with COVID-19 or the contact was wearing a cloth face covering.” Once exposed, the CDC recommends the exposed individual to “stay at home until 14 days after last exposure” and self-monitor symptoms – even if they test negative.
As for who should get tested, when contact tracing and testing is widely available (which it is not at the moment), the CDC guidelines include:
- Contact tracing will be conducted for close contacts (any individual within 6 feet of an infected person for at least 15 minutes) of laboratory-confirmed or probable COVID-19 patients.
- Testing is recommended for all close contacts of confirmed or probable COVID-19 patients.
- Asymptomatic contacts should self-quarantine and monitor for symptoms for 14 days from their last exposure (i.e., close encounter with confirmed or probable COVID-19 case), whether or not they test negative.
I don’t know about outside the SF Bay Area, but it is virtually impossible for me, as a pediatrician, to find a clinic or ER that will test an asymptomatic patient who has had close contact with a known or presumed COVID-19 patient. And even if tests were readily available with a reasonable turnaround time (I’ve seen turnaround times of 14 days!), the CDC still recommends that all close contacts quarantine for 14 days post-exposure.
The California Department of Public Health just published its COVID-19 and Reopening In-Person Learning Framework for K-12 Schools in California, 2020-2021 School Year on July 17, 2020. It notes that if there is a confirmed COVID-19 infection in a classroom, the school should:
- Identify contacts, quarantine & exclude exposed contacts (likely entire cohort) for 14 days after the last date the case was present at school while infectious
- Recommend testing of contacts, prioritize symptomatic contacts (but will not shorten 14- day quarantine)
Your child will likely be home for 14 days after classroom exposure –
even if they’re asymptomatic and test negative.
And let’s face it, in a classroom of elementary and middle school-aged children, even if their desks are spaced 6 feet apart and they are all wearing cloth face coverings, there WILL be “close contact” with a sick classmate. Have you ever tried to have a physical distancing playdate with your kids, whether they’re in preschool or in high school or any age between? We might as well call it physical magnetism… Even the California Department of Public Health has softened its COVID-19 Industry Guidance on physical distancing to recommend 6-feet distancing “if practicable.” And when that close contact occurs, the CDC guidelines infer that ALL of those children should quarantine for 14 days.
Even if children start school this fall in-person, they will likely spend more time quarantining out of school than learning in school. And while everyone is rightfully concerned about the socio-emotional impact of kids NOT going back to school, I have huge concerns about the socio-emotional impact of kids actually GOING BACK to school. With mask-wearing, physical distancing, no recess or lunch, it’s not clear how much socio-emotional benefit and joy learners will actually derive from being in school. And considering almost ensured stops and starts to in-school instruction due to post-exposure quarantines, these unpredictable disruptions may cause significant socio-emotional harm.
In order to reduce disruptions to in-school instruction due to quarantines, parents must COMMIT to being responsible and NOT sending their children to school when there is even a remote chance that they might be sick – with anything. The days of giving your child Tylenol before school so that child’s fever goes down and stays down for the entire school day are over. Symptom and fever checks may be useful in this regard, but nothing beats a mother’s spidey-sense when their kid is about to get sick. So if your spidey-sense is tingling, even if your child doesn’t have a fever or other symptoms yet, do your part and keep your child home.
Other countries who have reopened their schools have already witnessed these same starts and stops including Japan, South Korea, China, and Israel. France shut down its schools almost as soon as they were reopened after 70 new cases of COVID-19 were identified in school. This Summary of School Re-Opening Models and Implementation Approaches During the COVID-19 Pandemic dated July 6, 2020 shows that the highly-touted successful reopening of schools in Denmark and Norway without a significant increase in COVID-19 cases was due to low community transmission at the time of reopening – that is certainly NOT currently the case for the United States.
In areas of low community spread (which will require wearing masks, physical distancing, and flattening the curve), reopening schools likely SHOULD and CAN happen successfully. So if you would like your kids back in school soon, DO YOUR PART!
How is “low community transmission” determined? While it’s not a precise science, one of the factors to consider is the R0 (pronounced R “naught”) of COVID-19. The R0 value measures how easily an infection is transmitted, and predicts the potential for continued increase or decrease of that disease in a community. It basically is a measure of how many additional people, on average, a single person with COVID-19 will infect:
- If R0 < 1, each infected person spreads the virus to less than one other person. Case counts are predicted to decrease over time in that community and eventually fade away.
- If R0 = 1, each infected person causes one new infection. The number of cases in the community remains stable, but there won’t be big outbreaks.
- If R0 > 1, each infected person spreads the disease to more than one other person. The number of cases is predicted to increase exponentially in that community, with possible outbreaks or epidemics.
Michigan’s 2020-21 Return to School Roadmap, one of the most well-researched and thoughtful documents I’ve seen on how to reopen schools safely, recommends that schools NOT reopen for in-person instruction until the R0 is <1 and community cases are decreasing. At one point in time, the R0 of COVID-19 was predicted to be as high as 5.7. With inadequate testing and contact tracing, the true R0 value is difficult to calculate as noted in this article, but it has NEVER been below 1 in the United States.
We know a lot more about COVID-19 than we did back in February, and the mortality rate has significantly dropped from early estimates of what was seen in countries like Italy and Spain that were hit especially hard in the early days of the pandemic – this is GREAT! However, the fact remains that as cases continue to increase at alarming rates, people are still getting very sick, and our ICU beds are filling up and reaching capacity again – precisely the situation we’ve been trying to avoid, so that doctors don’t have to be in the same tragic position that they were in Italy of choosing which patients should get the critical care they need.
The curve has NOT been flattened.
A study in China found that social distancing was paramount to controlling the spread of COVID-19, and “although proactive school closures cannot interrupt transmission on their own, they can reduce peak incidence by 40 to 60% and delay the epidemic.” Earlier data from China in April found that school closures alone would prevent only 2-4% of deaths, so community measures continue to be important. And remember, flattening the curve doesn’t mean never getting COVID-19. Flattening the curve does mean slowing the spread so that our hospitals can manage cases and adequately care for patients in need.
The reality is:
Even if schools reopen their doors for on-campus learning in the fall, if the COVID-19 pandemic worsens in the winter months as predicted, I think lots of us will be back to shelter-at-home and 100% distance learning at some point this fall/winter.
So, while I would love more than anything to see all children back in school, Kenzi and Bodi included, I really don’t believe that most schools and communities are ready to open up for in-person learning anytime soon – in a way that keeps our educators and children safe and thriving, and in a way that is practical and sustainable.
There’s no one, right plan. We’ll all be learning from each other, watching how other schools are doing it, seeing what works and doesn’t work academically and socio-emotionally, and observing which schools have outbreaks or not. And we all must be prepared to be flexible, on a week-by-week basis.
If there is anything that this pandemic has taught us,
it’s that life must be taken one day at a time.
We all want schools to look like they did pre-pandemic. But they WON’T … at least not any time soon. And that’s the truth that we, and our children, must accept. It’s important that no matter how your child’s school decides to reopen, no matter how disappointed you or your child may be, that you remember:
Kids are RESILIENT.
Kids SEE the world through our lens. How positively or negatively we view an experience informs them how positively or negatively they should view that experience. School will reopen one way or another, and whatever the plan for your child’s school, they will remember this as a positive, or at least “OK” experience – IF WE DO, TOO.
Our school just announced that we would begin the school year with 100% remote learning with a phased plan for in-school instruction depending on community circumstances. And to my surprise, my first feeling was RELIEF. So many of us parents are in limbo right now, and we need informed leadership and wise decisions. Uncertainty creates the most anxiety. Before this announcement, though:
I had already decided that I would choose our public school’s 100% remote learning option and create our own “school pod” with a few of Kenzi’s and Bodi’s friends to stay connected socially and go through the curriculum together – even though Kenzi and Bodi both had COVID and may (hopefully!) have some immunity.
Yes, we are privileged to be able to choose this option. And I absolutely recognize that this is not a viable option for many families, YET. Not reopening school doors for in-person learning will have a disproportionately negative effect on children with special needs, our essential workers, working mothers, who during the pandemic have shouldered the brunt of child rearing and homeschooling, and many BIPOC and under-served families for whom school may be a necessary source of not just education but food and security.
But remember, we are almost assuredly going to be back to sheltering-at-home at some point this winter, and schools, childcare centers, and employers MUST be prepared to ensure the physical, socio-emotional, academic, and financial health of ALL of our children and their families. Whether or not school starts in-person in the fall, the time is NOW to figure out how to optimally support ALL of our children with a robust distance learning program that also fosters socio-emotional development and peer connection in a way that supports each families’ unique needs. And those schools that start with remote learning may have a leg up…
What about schools that are planning to re-open their doors to in-person learning?
How truly safe is that for our children and our educators?
Many schools are basing their decisions on the answers to 2 very important questions – the answers to which are still not clear but are absolutely critical to informed public health and education policy:
- Do children get seriously sick from COVID-19?
- Can children spread COVID-19?
THE PROBLEM: the data is LIMITED. Our children have been quarantining at home since shelter-in-place orders in March, and continue to be largely shielded from the outside world and coronavirus exposures. Most parents are still not taking their kids on Target or Costco runs like they did pre-pandemic (which might be a relief for some!). To say that kids don’t really get COVID-19, and don’t really get that sick from COVID-19, is a hopeful statement (I would LOVE for that to be true), but not based on an abundance of good data. As children re-enter society, we expect to see an increase in pediatric COVID-19 cases, just as we’ve seen an increase in cases in young adults as they have re-entered society. And with this increase in cases, the answers to these questions will become more clear.
Let’s look at the data we have so far, because to every extent possible, schools need to base their reopening decisions on the evidence at hand. The American Academy of Pediatrics issued a joint statement on July 10, 2020 along with the American Federation of Teachers (AFT), National Education Association (NEA) and The School Superintendents Association (AASA):
“Returning to school is important for the healthy development and well-being of children, but we must pursue re-opening in a way that is safe for all students, teachers and staff. Science should drive decision-making on safely reopening schools. Public health agencies must make recommendations based on evidence, not politics. We should leave it to health experts to tell us when the time is best to open up school buildings, and listen to educators and administrators to shape how we do it … schools in areas with high levels of COVID-19 community spread should not be compelled to reopen against the judgment of local experts. A one-size-fits-all approach is not appropriate for return to school decisions.”
Do Children Get Sick from COVID-19?
New pediatric data from Florida as of July 10, 2020, where they are seeing a skyrocketing number of new daily cases, reported that 31.1% of children tested were positive for COVID-19 – 16,797 children with COVID-19 out of 54,0222 children tested. That means 1 in 3 children tested were positive for COVID-19 – much higher than the 11% positive rate in adults in Florida. Cases were about evenly split between those children over 10 years (55%), and those under `10 years of age (45%).
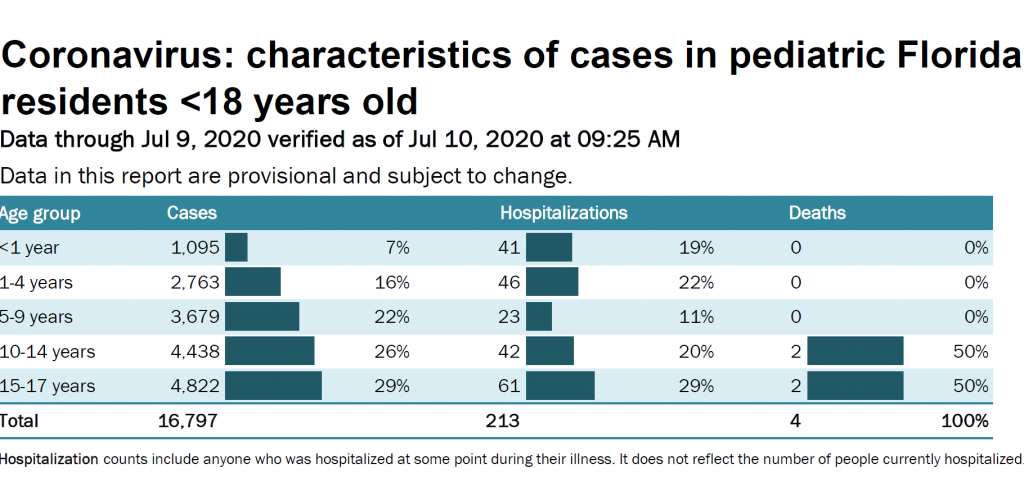
The most recent US data on COVID-19 cases by age is from May 30, 2020 – which in “COVID time” is a lifetime ago. Between January 22 and May 30 ,2020, children 0-19 years made up approximately 5% of all laboratory-confirmed cases. That number is likely higher now. Data from California show that as of July 18, children <18 years represent 8.6% of all COVID-19 cases, but testing continues to remain woefully inadequate.
Kids obviously do get sick with COVID-19, and as children face more exposures with school reopenings, and testing becomes more widely available, this percentage will likely rise.
The data so far reassuringly shows that the vast majority of kids tend to do well when sick, sometimes get hospitalized and need ICU care, and rarely die.
Why children seem to get “less” sick from COVID-19 has been puzzling, as this is not the case for many other viral infections like influenza. The answer may lie in the ACE-2 receptor. In my article, Kawasaki Disease, ACE-2 & COVID-19, I describe how SARS-CoV-2 virus enters cells through ACE-2 protein embedded in the cell membranes of many of our organ systems (“functional” ACE-2 receptors). This recent JAMA study measured ACE-2 gene expression in the nasal passages of children and adults, 4 to 60 years old. Researchers found that children <10 years of age express significantly lower amounts of ACE-2 in their nasal passages than older children 10-17 years, young adults 18-24 years, and adults 25 years and older, with nasal ACE2 gene expression increasing in each age group.
CONCLUSION: Young children under 10 years of age may be less at risk for contracting COVID-19 and developing serious infection.
IMPLICATION FOR SCHOOLS: Reopening in-person instruction for preschool and elementary school-age children may be lower risk for children.
On the other hand, some children will get very sick. While death and serious complications like Multi-System Inflammatory Syndrome in Children (MIS-C) are rare, they are never to be taken lightly. As cases increase around the country, there are also increases in cases of MIS-C being reported in recent weeks, including in Florida, Wisconsin and South Carolina. And we have no data on the long-term complications of COVID-19 in children, including lung scarring and blood-clotting abnormalities, that may persist even for children with mild or asymptomatic disease. I will be looking closely for this data as it emerges.
Do Kids Transmit COVID-19?
I’ve heard many people comment that even if kids get it, they don’t spread it. So, if kids don’t get infected that easily, don’t get sick as often, and don’t transmit COVID-19 as frequently, then perhaps we should reopen school regardless of community spread since educators, parents and grandparents won’t have to worry as much about students giving COVID-19 to them.
Let’s look at some of the most recent data we have, because from a public health perspective, how kids transmit COVID-19 may be the most important question to answer.
Initial studies speculated that children were not big spreaders, especially young children. A Dutch study in March 2020 of 54 households with confirmed COVID-19 found that children under 12 were less likely to have COVID-19, and concluded that transmission appeared to be primarily between adults, and from adults to older children in the same household. There was a frequently-cited case of a 9 year-old French boy with COVID-19 who did not transmit the disease to more than 170 known contacts.
But more recent reports point to concerns that children may indeed spread disease, even if asymptomatic. A rigorous large new study from South Korea, where contact tracing has been extensive, found that children, especially older children 10-19 years of age, spread COVID-19 at least as often, or more often, than adults. Children under 10 years were about half as likely to transmit COVID-19. The average rate of COVID-19 transmission across all ages was 11.8%. Surprisingly, children 10-19 years had the highest COVID-19 rates of transmission any age group – 18.6% of their household contacts tested positive. Children 0-9 years with COVID-19 had the lowest rates of transmission – 5.3% of their household contacts tested positive. Better, but still not zero.
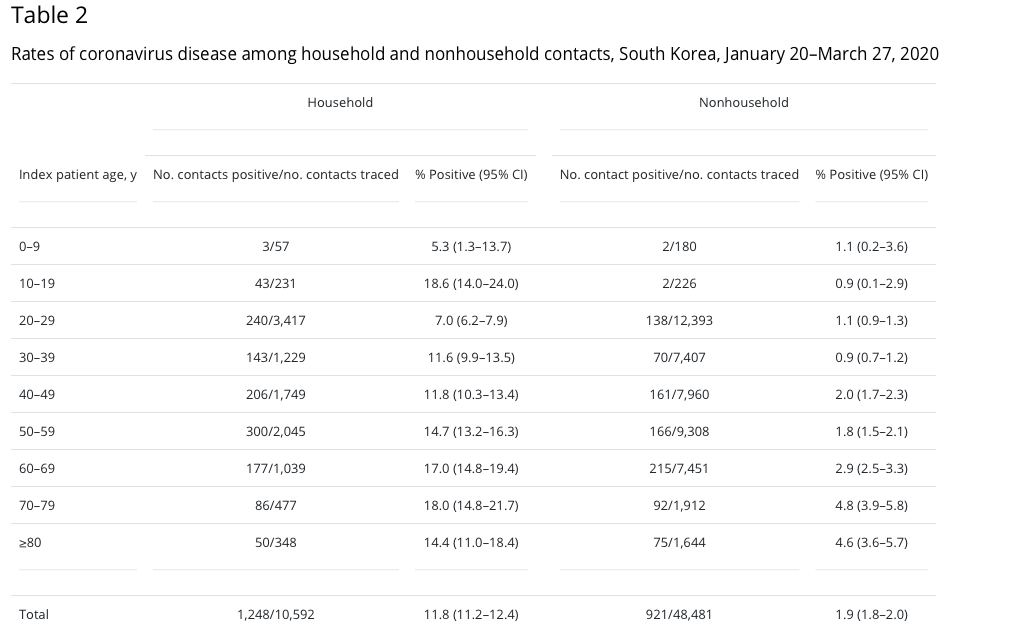
CONCLUSION: Young children under 10 years of age may be less at risk for transmitting COVID-19 to close contacts.
IMPLICATION FOR SCHOOLS: Reopening in-person instruction for preschool and elementary school-age children may be lower risk for educators and school staff.
The Korean study only looked at symptomatic children and adults. Given that as many as 40-45% of patients may have asymptomatic disease, it is also important to know whether asymptomatic children can spread infection. The answer to this is not entirely clear. However, a German study analyzed 47 children ages 1-11 years infected with SARS-CoV-2. Children who were asymptomatic had viral loads that were as high or higher than symptomatic children or adults. While this does not tell us how contagious asymptomatic children are, many studies show that a person’s viral load is closely tied to how infectious that person is. If this is the case with COVID-19, asymptomatic children may pose a higher risk to their classmates, educators and school staff, and household members than previously thought.
Socio-emotional, Academic, Equity & Other Concerns
The decision to reopen schools is not just about whether our kids, their families, and educators will get COVID-19. There are socio-emotional considerations. There are academic considerations. There are equity considerations. And there are non-COVID health concerns.
Young children in particular need peer interaction for optimal socio-emotional, behavioral, and speech/language development. The academic skills learned in grades K-2 set the foundations for future success in all subject areas. Young children in particular will have challenges sitting through online Zoom sessions – have you ever tried to FaceTime the grandparents with your 5-year-old?
For middle-school and high-school students, peer interactions become an essential part of their social development and emerging self-identity. Students are experiencing high levels of anxiety and depression due to the quarantine, and if continued lockdowns and school closures are a necessary part of keeping our communities safe, schools must find creative ways for students to stay socially connected and ensure that physical distancing does NOT mean social distancing and social isolation.
Children with special needs will likely be best served by in-person instruction and should be prioritized for safe return to school. If your child has ADHD, autism, dyslexia or learning difference, there is a very real concern that the academic gap will widen and they will fall further and further behind their peers.
Children in rural areas and underserved populations may have limited access to computers and internet access with enough bandwidth to support remote learning.
Families with working parents, especially single parents and essential working parents, must be prioritized for safe, in-person instruction, and must be supported by their employers with flexible work schedules, and job and financial security. The unacceptably high rates of joblessness must be addressed at a larger policy level.
Meal service providers must ensure that systems are in place to ensure that no child is hungry. A national Survey of Mothers with Young Children conducted in April 2020 found that 40.9% of mothers with children 12 years and under reported that their children did not have enough food to eat. US Census Bureau data from May 28-June 2 found that more than one-third of SF Bay Area households reported a lack of consistent access to affordable, healthy food.
We also must consider whether schools are structurally ready. Schools, especially those in urban and underserved areas, may not have the physical space to keep children 6 feet apart or hold classes outdoors. Given the increasing evidence for airborne transmission of COVID-19, schools may not have, or be able to afford, updated HVAC ventilation systems that minimize recirculating air, accommodate HEPA filters with adequate MERV ratings or have UV light technology that may reduce potentially infectious aerosolized particles.
The huge increase in screen time that school shutdowns have caused must also be addressed, for our younger and older students, with the resulting impact on anxiety/depression and potential lifelong implications for their developing brains. The Adolescent Brain Cognitive Development (ABCD) study is the largest long-term study of brain development and child health in the US that started in 2016, following over 11,000 children ages 9-10 years of age into early adulthood. Brain MRI scans of 4,500 children found significant “cortical thinning” (i.e., brain shrinkage) in children using digital devices for 7 or more hours/day (check your, and your child’s, screen usage – trust me, 7 hours is easier to do than you think). Children using 2 or more hours/day of screen time had lower scores on thinking and language tests. While FaceTime, texting, social media, and internet games are an important way for children to stay connected socio-emotionally while physically distancing, the harmful effects of screen time must be balanced with the necessity of remote learning, and schools must think creatively about how they will present their curriculum to students, allowing for some non-screen learning and assignments.
Daily movement/exercise and optimal sleep hygiene must also be encouraged and prioritized by schools. The children in my practice who I saw doing better during school closures were the students whose schools maintained an online curriculum that mirrored their in-school schedule, with consistent start, end and break times. Predictability and routine are key for children to successfully navigate remote learning with minimal anxiety and stress. School attendance check-ins must be daily and required, so that children wake up at a consistent hour on school days, and hopefully go to sleep at a consistent hour on school nights. Even if the total number of hours seems adequate, going to bed at 3am and waking at 1pm is NOT a healthy sleep pattern that will optimize brain function and immune resilience during the pandemic. As part of this consistency, schools must maintain and require adequate movement and outdoor time each day. Too many children in my practice did not move their bodies every day, and some spent days without stepping a foot outdoors.
Optimizing sleep and exercise are critical for supporting our immune systems during the pandemic. An increase in sleep actually increases the number of your white blood cells. On the other hand, loss of sleep even for a few hours at night, increases inflammation in our body which makes us more susceptible to catching the flu and having more severe symptoms. Lack of sleep also exacerbates any attention/focus and behavioral concerns your child may already have. Moderate exercise can boost the production of macrophages, the kind of white blood cells that “eat” bacteria and viruses. However, intense exercise can actually temporarily decrease immune function – so don’t overdo it!
So, what’s my bottom line?
I fully support the reopening of schools – when it is SAFE(R).
In-person instruction is absolutely the ideal situation for children – as long as it doesn’t put their health, or the health of those around them, at risk. In the meantime, while most communities experience continued rates of increase in COVID-19 cases, remote learning should be offered while ensuring the socio-emotional, academic, and financial security of all children.
When community spread is consistently on the decline, schools should re-open, beginning with our younger children under 10 years of age, who may be at lower risk for contracting COVID-19 and having serious complications, and may be less likely to transmit infection to more vulnerable school staff and family members.
In-person instruction should also be prioritized for special needs and underserved children for whom distance learning may not be feasible or safe for a variety of reasons.
But remember, the risk to educators and students of contracting COVID-19 will never be zero, even once community spread begins to decline. We can’t wait for zero risk. Our children, our parents, and our economy need schools to be open.
While the risk of infection remains, it is imperative to support our immune systems to be as resilient as possible. By the time this pandemic is over, the majority of us will have contracted COVID-19. If it’s a matter of WHEN, not IF, we will contract COVID-19, we must do everything we can to ensure that our children’s, and our own, immune systems are the least friendly host to the SARS-CoV-2 virus possible – that is what immune resilience is all about. The ability to contract an illness and bounce back quickly and fully, to be even stronger for the next hit. With an integrative and functional medicine approach to the pandemic, immune resilience is entirely possible. To get you started on understanding how to optimize immune resilience during the pandemic using food as medicine, diet & lifestyle, and targeted supplements, I’ve created the following resources for you based on my experience, clinical knowledge, and research as an integrative pediatrician and pediatric functional medicine expert.
COVID-19 RESOURCES:
- Article: A Pediatrician’s Pandemic Immune Support Plan
- Article: Kawasaki Disease, ACE-2 & COVID-19: what a pediatrician wants you to know
- FREE Masterclass: A Holistic Pediatrician’s Guide to the Pandemic
- Online Program: Integrative & Functional Medicine Strategies for the Pandemic
And be sure to stay tuned for my upcoming article on Preparing Your Child to Return to School Safely, to learn how to minimize your child’s risks as their schools reopen for in-person instruction, whenever that happens.
Stay well … we’re all in this together!
xo Holistic mama doc – Elisa Song, MD
Thank you. Thank YOU!!!!
You’re so welcome! xo
I think like you do. My children are grown but we got measles shots, TB and diphtheria shots
How tremendously helpful. Thank you, Dr. Song!
you’re so welcome, Katie! xo
Thank you THANK YOU for such an incredibly well thought out post on what Has been weighing on me (and many/most) for weeks. So appreciative
Yes, it’s been weighing on all of us for week. So grateful I can help sort out some of the issues! xo
I’m in NJ and currently our transmission rate is 0.8….. our town hasn’t released plans yet. But neighboring towns are Planning for K-5 to attend every day, half days (4 hours), no lunch or eating at school. Class size will still be close to 20 kids per class. Curious if you have any thoughts …..
WOW! Thank you sincerely for taking the time to write this up. Super duper helpful and encouraging as we navigate these upcoming months and remainder of this crazy 2020 year! You are incredible and a valued resource to society.
Thank you so much, Robin. So glad you found it helpful! xo
Thanks a lot . As always your perspective on all this is something I look forward to. Thanks for all the contribution to our community
you’re so welcome! xo
Thank you! As always, I appreciate your thorough research and thoughtful approach. One burning question: you did not mention anything about whether you think wearing masks for hours a day is safe for children. I have read and heard some say that it can lead to other health issues, and others say that the safety of mask wearing in children has never been studied in children and, thus, should not be recommended or mandated. As a psychotherapist, I also worry about the social-emotional impact of mask wearing in children, especially for caregivers wearing masks around babies and very young children who are wired to read facial expressions and the movement of mouths in order to form secure attachments to caregivers and learn to talk! I would love your thoughts on this.
Hi Allie – I am diving into mask research and my next article will be about Masks & Children so stay tuned! xo
That would be great— you are a terrific resource!!
Do you have a list of recommended supplements to keep kids at their peak health during all of this?
Hi Brindi – yes! Definitely listen to my free masterclass and read my article on pandemic immune support that I list at the bottom of the article. There are a ton of useful resources there. Stay well!
Thank you Dr Song. I trust your brain so much!
thank you, sherry! xo
Muchas gracias dra. Song!!
De nada, Ana! xo
Thank you, Dr. Song, for another well-researched article. As a teacher and mom to two young kids, (my oldest is about to start Kindergarten at my school), the question of reopening schools either in-person or online has given me the most anxiety since we closed our school in March. On the one hand, as a teacher, it is literally my job to provide quality education and to look after the wellbeing of my students. On the other hand, facilitating lessons live via Zoom negates my ability to supervise/set up/assist my daughter as she attends her own live Zoom class. (My husband is a teacher too). This leaves us in the impossible position of having to be in two places at once. All this to say that there are so many different things to consider when schools begin to reopen.
so many things to consider, and there is no ideal solution. you have 2 of the most important jobs of all. stay well!
Thank you, Dr. Song! Your tireless efforts and sage words are a bright spot in these uncertain times. I appreciate that you are an evidence-based, reliable source of information.
thank you so much! I appreciate your kind words!
My nephew is attending summer classes in his primary school as he has special educational needs, it is important that he gets some support in learning after many months of quarantine during the lockdown began and that he can also get exercise leaving for the outdoors essentially.
special needs kids absolutely need to be prioritized for in-school learning…
Great article. Thank you for your perspective!
you’re so welcome!
Hi, with schools in my area most likely going 100 percent distance learning through January , what are your thoughts on sports activities. I have 2 Very active boys, who with distance learning will be on the house all day and need intense physical exercise to maintain behavior and emotional well being. With winter approaching our option for many hours of running and playing outside will significantly decrease. What are your thought on group exercise outside of the home. I am considering signing them up for gymnastics (will be a group of 6 children)My boys really need physical activity and it’s hard for me to provide the duration and intensity they need within the home. I know this is long, but this has been a recent discussion between my friends and family.
this is such an important question. my son has been lucky enough to have his sister and our neighbors kids’ as their “pod” to run around with, jump on the trampoline, and go on bike rides – and it’s still not nearly as much activity as when he was in school. I think that if it’s a stable cohort of kids, the studio is cleaning equipment thoroughly, they can open windows for ventilation, and your sons are good about keeping their hands away from their faces and washing hands – it could work and be so important for their mental and physical health. Good luck!
Thank you so much for your input !!!!
This is so wonderful. Will be sure to send to some of my concerned friends here in NC!
so glad you found it useful!
Dr. Song, thank you for your empathy and generosity–so appreciate you thoughtfully taking time to share this!!
You’re so welcome – stay well! See you soon!
You have been such an incredible source of quality information and comfort for me during this crazy time! Thank you thank you for all you do!
you’re so welcome! I’m so grateful that you’ve found my information useful. xo
Dr. Song- thank you for all you do! Hugely useful article – and helpful as we all navigate these next few months as parents!
I’m curious if you’ve read any of Doris Loh’s research – she believes that doctors/scientists have inaccurately identified ACE-2 as the functional receptor, instead of cd147.
Here’s some of her research: https://www.melatonin-research.net/index.php/MR/article/view/86/568?fbclid=IwAR24dj725gJPml3SpQBjHZ6kMi5P_YKDRVLnKVyW6S20gZlON-y1CEZc3tU
Thank you, Lisa. And yes – Dr. Loh’s is very interesting. It doesn’t replace ACE2 as a target. The ACE2 enzyme is still the functional receptor for the SARS-CoV-2 virus on the cell membranes of various organs including the lungs, GI tract, kidneys. The CD147 functional receptor is located on red blood cells and T-cells, which may account for the blood-clotting complications that are being seen in some. The common pathway to cytokine storm whether triggered by the ACE2 or CD147 pathways is the NLRP3 inflammasome, and melatonin is actually an immune modulator that may be beneficial to regulate the NLRP3 inflammasome regardless of cause. Fascinating! I am working on an article to explain both of these mechanisms and what we can do from a functional medicine standpoint…
I’m in South Africa. Our schools went back for 3 weeks and we’re about to close again this week due to the high number of cases. My kids adjusted so well in those 3 weeks. They had to wear masks, socially distance and sanitize. They were just so happy to be back with friends. Even my older son who is 8 and ADHD and usually struggles with change and anxiety was thrilled to be back and coped really well. He still managed to pick up a head cold 2 weeks in, which as you say all the measures are not effective. But as his teacher said to me, it is us adults who find it hard to adjust, she said all the kids were coping well. Its important to speak to them about their fears. He needed reassurance when he got sick, about not every illness being Covid and that even if he did get it his immune system is strong and we would get through it.
Thank you for all your advice Dr Song. xxx
This is SO important for us to remember, Sheryl! Even watching kindergartners go back to abbreviated summer programs, the masks were hard for about a day or two and then they were absolutely fine with it AND having fun with their peers. We as parents project so much of our own fears and worries about how kids will handle masks, physical distancing and sanitizing that we forget how resilient kids can truly be. xo
This is one of the best POVs I’ve read about returning to school during a pandemic. Thank you.
Thank you so much, Idil – I’m so grateful that you found it usefl!
Such a helpful article. Thank you so much!
You’re so welcome, Lisa!
Thank you Elisa!!! So balanced, I hope every parent reads this!
thank you, Paula!
This is the most well thought-out, fact-based article on this topic that I have read. I passed this along to all the parents of school-aged children I know and posted it on my FB page. Thank you for writing such an incredibly resourceful article. You have enlightened so many people on the facts and provided them with your professional opinion to help them navigate these difficult decisions. Thank you Dr. Song!
Thank you so much, Vicki! xo
You always provide the most detailed, thoughtful, and well-researched information! Thank you!
thank you!
Hi – As someone who has a leadership role in whether or not we reopen our districts schools this fall, I really appreciate this article. It gave me a lot of thing to think about and some real ideas to implement. I am a numbers person so have a few thoughts too. The age range of 10-19 seems like a large and vastly different population to base the assertion that older kids spread the virus. I wish they could have broken that by middle school kids vs high school aged students. Also, when I look at the percentages of how many these students spread it to, although higher in the older kids, it still is very low. For a family of four with a spread rate if 18.6% that is not even one person they spread it to (only .75). Just some thoughts and would be happy to hear any additional thoughts you have. Thank you again!
These are all great thoughts. I also wish the data had been broken down further into middle and high school blocks. You’re right – the transmission rates are not very high, which is why so many other factors need to be taken into account. Good luck with your decisions. I’d love to hear what your school district decides to do and how you came to that decision. Good luck!
Thank you so very much for this. Have you come across any data about infection risk even if staying 6ft away (mask or no mask) for hours at a time in an enclosed space (ie like a classroom)? I’m craving this info. thanks!
Hi Mary – I haven’t come across this data specifically. We know that wearing masks, physical distancing, and being outdoors can reduce the risk of infection. Unfortunately, I haven’t seen any studies that manipulate each of these individual factors. So needed!
Dr. Song, I wonder if you have any suggestions on outdoor class once a week? Would it be a safer option to consider? With one teacher, one adult parent helper and about 10-12 kids. Physically distance and have mask or non mask.
Thank you.
Thanks for this article Dr. Song! If you were to move somewhere in the USA where schools are most likely to remain open for in-person instruction, where would that be? Florida because they are closest to herd immunity? Or somewhere like South Dakota because they are the least locked down and don’t have any surges? Or somewhere else?
Also, any tips for places where school pods are only allowed with 6ft distance at all times and masks, both indoors and outdoors? Is there actually much beneficial social interaction under these circumstances?
Many thanks in advance for your thoughts.
Hi Susan – it would definitely not be Florida. While their numbers are skyrocketing, they’re still not anywhere near herd immunity, which likely will require at least 70% of the population having been infected. You may be right – it may be rural areas with very low population density that right now has the best chance to open “normally.” As for beneficial social interaction with social distancing and masks – as I said, kids are so resilient. I’ve had kids return to daycares, summer school programming and camps with public health measures in place – and parents had the very same concerns. While some kids had a really hard time the first day or two, within days I heard from parents that they had adjusted and were having a great time with their friends…
Thank you so much for such a comprehensive, well thoughtout and researched article. I truly appreciate it and know others do as well!
You’re so welcome!
This is fantastic piece Elisa! The most thorough, thoughtful and informative I’ve read on the subject.
We too felt relief when our 15 y.old son’s school district announced a complete turnabout with distance only learning this fall following governor Newsom announcement. The situation had put us patents in conflict with him about partial school I striction versus full distance learning, albeit we were fully supportive of with outdoor cross country running team in small groups.
Grateful we don’t have to be the unfair bad guys and can focus on parenting.
Outdoor time and over doing media in all forms is our biggest concerns for our teenagers well being since we are spared most other concerns (aside from Covid of course.) I’ll make sure to show him the study about cortical shrinking – that should strike a cord.
Thank you for taking time to write and share this Dr Song.