Could your child have PANS/PANDAS?
Do you have a child who was totally “normal” one day, and the next day suddenly has new anxieties, fears, tantrums or rages, OCD behaviors and maybe even tics? Does your toddler have out-of-control tantrums, and your friends and parents think you may have parenting issues? Or do you have a child who has always been more anxious, but now has gradually worsening separation anxiety and mood swings, who used to be a great student but is now barely holding on because she can’t focus and has difficulty processing or remembering what she’s learned just the day before?
Are you thinking, and hoping:
It’s just a phase …
It could be, but it could be something more … it could potentially be an autoimmune illness that is affecting your child’s brain – something called Pediatric Acute Onset Neuropsychiatric Syndrome (PANS) or Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Disease (PANDAS).
According to the American Academy of Pediatrics, at least 1 in 200 US school children has PANS (1), and that number is climbing every day, but many are misdiagnosed, or just plain missed.
Missed Diagnosis – Missed Opportunities
According to the PANDAS Parent Survey in April 2014 (2), it took over 3 years for 35% of children to be appropriately diagnosed with PANS/PANDAS. Almost 90% saw 3 or MORE doctors before being properly diagnosed. Over half of all children with PANS were misdiagnosed and mistreated for over 1 year. Most children are misdiagnosed as having psychiatric illness, behavioral problems, or parenting concerns. Many go through trials of multiple psychiatric medications and therapies with minimal to no benefit – because they’re treating the WRONG thing.
PANS is so much more than a “mental health disorder.” PANS/PANDAS is an immune-modulated, neuro-inflammatory encephalitis. What on earth does that mean?
Our kids’ brains are on fire!
Without appropriate antimicrobial, anti-inflammatory, and immune-modulatory treatments, our children with PANS/PANDAS will be facing an uphill battle in their fight to get well and heal their brains.
Unfortunately, by the time many children get the treatment they so desperately need, they’ve likely already been misdiagnosed and mismanaged. It is imperative that pediatricians, family practice doctors, pediatric occupational/physical/speech therapists, psychologists, psychiatrists and educators understand what PANS/PANDAS is. Providers who care for children play a vital role in recognizing how children may present with PANS/PANDAS so that they can be appropriately referred, diagnosed, and treated as soon as possible.
Only then is recovery possible.
What is PANS/PANDAS?
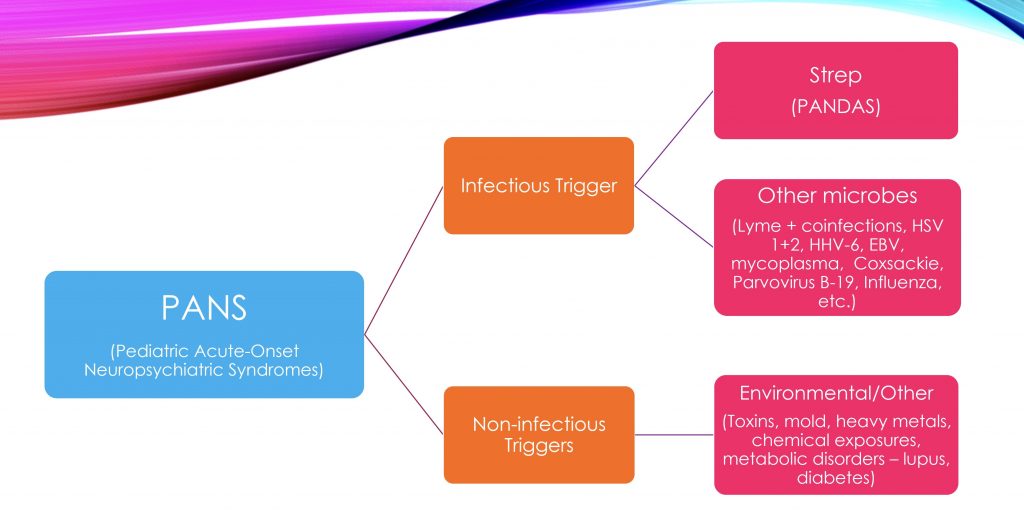
PANS (Pediatric Acute-onset Neuropsychiatric Syndrome) is an autoimmune encephalitis that can have multiple triggers – infectious and non-infectious. Infectious triggers appear to be more common than non-infectious triggers. PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Disease) is a subset of infection-triggered PANS caused by streptococcal infection. However, many infections are now known to be possible triggers of PANS including Mycoplasma pneumonia, Influenza, Epstein Barr Virus, Lyme and other tickborne coinfections, HHV-6, HSV 1+2, Parvovirus B19, Coxsackievirus, Cytomegalovirus, and Candida. Non-infectious triggers include environmental toxins such as mold, heavy metals, and other toxic exposures, as well as metabolic disorders such as diabetes and lupus cerebritis. This diagram gives a better picture of how to think about PANS and all of its potential triggers.
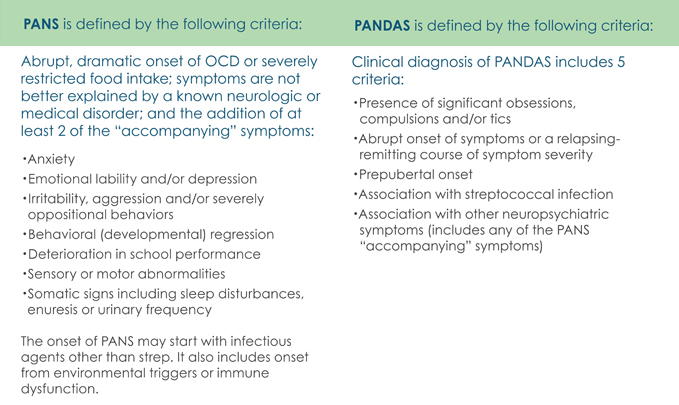
How is PANS diagnosed?
The following are the current diagnostic criteria for PANS/PANDAS:
Symptoms of PANS/PANDAS can vary quite a bit, and the most common symptoms that I typically see in my patients include the following:
- Dilated pupils
- Anxiety
- Separation anxiety
- Behavioral regression (baby talk, watching cartoons from when they were younger, etc.)
- Obsessive-Compulsive symptoms
- Tics (vocal and motor)
- Extreme mood swings/emotional reactivity
- Rages/tantrums
- Difficulty focusing
- Slower processing speed (harder time understanding questions and concepts)
- Poor short-term memory (doesn’t remember what they learned just the day before)
- Handwriting decline
- Food restriction (fear of choking, throwing up, contamination, etc.)
- Hand tremors
- Clumsiness
- Heightened sensory issues (can’t stand certain sounds, smells, textures)
- Urinary changes (frequent urination, feeling as though they always have some urine left)
- Sleep difficulties
Not always abrupt and dramatic …
While the current diagnostic criteria require an “ABRUPT, DRAMATIC ONSET” of symptoms, in my clinical experience and the experience of many other integrative and functional medicine practitioners – there are many children with a more “subacute” onset of symptoms. There’s a CHANGE somewhere in the past. Parents feel that their kid is different EVER SINCE some event. Maybe it was A CHANGE in mood, anxiety, sleep, focus/attention EVER SINCE the birth of a baby brother, or starting a new school, or after a divorce. A CHANGE that you think is “just a phase,” except the phase doesn’t end.
Consider the possibility of PANS/PANDAS whenever you find yourself thinking your child has changed, ever since …
If you don’t look, you won’t know, and yet another child will be missed…
Is There a Test for PANS/PANDAS?
PANS/PANDAS is a clinical diagnosis.
That means that there is no single test that will tell you if your child has PANS/PANDAS. Diagnosis starts with clinical suspicion.
While PANS remains a clinical diagnosis, the goal of testing is to determine the root causes(s) for why your child’s brain is on fire in order to better customize treatments.
Clinical history should be the guide as to which tests to run first.
Did your child have recent or recurrent strep infections in the past? Know that strep infections do not always present as classic strep throat. Kids can have strep in their throat, on their skin (impetigo), colonized in their noses, or as a bright red ring around their anus (perianal strep). Blood tests may reveal persistently elevated anti-streptolysin O (ASO) and anti-DNAse B strep antibody levels.
Did your child have any other infections that you remember may have occurred shortly before their neuropsychiatric symptoms appeared? Does your child get frequent cold sores? Do you hike in nature and enjoy camping as a family – could there possibly have been any tick bites in the past? Have you had any water damage in your home – could your child have been exposed to mold or mycotoxins? Any other possible toxic environmental exposures?
Quantitative IgG and IgM antibody levels should be assessed for possible infectious triggers of PANS, as indicated by clinical history or suspicion. These may include testing for Streptococcal infection, Mycoplasma pneumonia, Influenza virus, Epstein Barr Virus, Lyme and other tickborne coinfections, HHV-6 (the roseola virus), HSV 1+2 (the “cold sore” virus), Parvovirus B-19 (the “slapped cheek” virus), Coxsackievirus (the “hand-foot-mouth” virus), Cytomegalovirus, Candida, and potentially others as indicated by your child’s history. IgM antibodies reflect recent or active infection. IgG antibodies reflect past infection. However, it should be noted that the presence of elevated IgG titers may represent persistent chronic active infection despite negative IgM titers. While under-recognized, this phenomena was noted as early as 1991 with severe chronic active Epstein-Barr virus infection syndrome (3). Targeted antimicrobial treatment should therefore still be considered for a child presenting with neuropsychiatric symptoms and very elevated IgG titers despite negative IgM titers.
If all antibody levels are negative and no infection is detected, non-infectious triggers must be considered. Appropriate testing should be performed as indicated by clinical history for mycotoxins, heavy metal exposures and other toxic exposures.
Despite the above testing, there will be children with PANS who do not have clearly identifiable triggers. For those children, the “Cunningham panel” offered through Moleculera Labs (4) in the United States can be a valuable piece of the diagnostic puzzle. The Cunningham panel, developed by immunologist Dr. Madeleine Cunningham who has been on the forefront of PANS research, tests for 4 neuronal auto-antibodies – these are antibodies against parts of your child’s brain (Anti-Dopamine Receptor D1, Anti-Dopamine Receptor D2L, Anti-Lysoganglioside GM1, and Anti-Tubulin) as well as activity of the CaM Kinase II enzyme (Calcium-dependent Calmodulin Protein Kinase II) found to be elevated in patients with PANS.
“Conventional” Treatment Approaches to PANS/PANDAS
Treatment guidelines for the Clinical Management of Pediatric Acute-Onset Neuropsychiatric Syndrome were published in the Journal of Child and Adolescent Psychopharmacology in July 2017. “Conventional” treatment for PANS incorporates 3 arms – psychiatric/behavioral interventions (5), immunomodulatory therapies (6), and antimicrobials to treat and prevent infection (7).
From a behavioral and psychiatric standpoint, it is critical that children work with a psychologist or psychiatrist who understands what PANS/PANDAS is. Even in the San Francisco Bay Area where I practice, just down the street from the Stanford PANS Clinic, there aren’t enough psychiatrists who really understand what PANS/PANDAS is. In fact, there are still too many psychiatrists who are skeptical that PANS/PANDAS even exists!
I have a beautiful girl in my practice with PANDAS who is now thankfully recovered.. Her family moved away when she was in elementary school and returned during middle school. She had been at the top of her class academically, loved by everyone socially, and a star competitive athlete. When she moved back, I barely recognized her. She had started cutting, and had extreme anxiety and OCD symptoms. Her pupils were widely dilated, heart racing, hands tremoring, and she had bruises all over her shins because she had become so clumsy. She was failing academically because she just couldn’t understand what was being taught. And if she did understand one moment, it would be gone the next. When I asked her questions, she would stare blankly at me, trying to understand what I was asking her, until she finally got it and slowly began to answer. Her psychiatrist had placed her on 2 different psychiatric medications – neither of which was really helping. I knew she was a different kid in front of me than the kid I had known years before. So I ran multiple tests, and found that she had very elevated strep titers. I started her on antibiotics and other functional medicine supports, and within 4 weeks, her mother called and said:
“She’s back.“
Within 8 weeks, we were able to wean her off her psychiatric medications. She went back to her psychiatrist and told him what had happened, and his response was:
“You don’t have PANDAS.“
Because it didn’t have an acute and dramatic enough onset. Because she doesn’t fit the “classic” PANS criteria. And because he’s not even really sure that PANDAS exists …
School accommodations must be in place so that parents are immediately notified of infectious diseases that may trigger a PANS/PANDAS flare in their children. Educational adjustments must be made with an understanding of the waxing and waning nature of PANS/PANDAS. There will be weeks where children will be completely neurotypical, emotionally regulated and performing beautifully in school, and weeks where these very same children will have debilitating fears, OCD symptoms, tics, memory and cognitive processing issues, severe handwriting decline and extreme mood swings.
Cognitive behavioral therapy (CBT) and family therapy are important adjuncts to any medical intervention. If access to a qualified CBT therapist is unavailable, Dr. Dawn Huebner’s books cited below are invaluable tools to teach children and teenagers CBT techniques to manage their anxieties and OCD. Psychiatric medications may be necessary in times of crisis for severe OCD, anxiety, depression, ADHD symptoms, sleep disturbance, and other neuropsychiatric symptoms. However, these medications and behavioral interventions are only band-aids, and often not as effective as hoped until the underlying neuro-inflammation, infections, immune dysfunction, and other core clinical imbalances are addressed.
Anti-inflammatory and immunomodulatory treatments are often required in order calm the fire in kids’ brains, protect the brain and provide symptom relief in order for healing to take place. These therapies may include Nonsteroidal Anti-inflammatory Drugs (NSAIDs), oral and/or IV steroids, monthly high-dose Intravenous Immunoglobulin (IVIG), therapeutic plasma exchange or plasmapheresis, and IV rituximab. These treatments are designed to suppress the immune system, but do not address the underlying immune dysregulation that caused your child’s immune system to attack their brain in the first place.
Antimicrobial treatment and prophylaxis are critical in the management of PANS/PANDAS. Conventional antibiotic guidelines are more defined for the treatment of acute streptococcal infections in patients with PANDAS. The benefit of long-term antibiotic prophylaxis is less clear; however, most children do seem to benefit from prophylactic antimicrobials to reduce the likelihood of a PANDAS flare after repeat strep exposures.
There are fewer guidelines for the management of PANS triggered by non-streptococcal infections like viral infections or Lyme and other tickborne infections, and even fewer still for non-infectious PANS triggered by mold, heavy metals or other toxic exposures. For non-strep PANS triggers, working with an experienced functional and integrative medicine doctor is key.
The “conventional” treatment of PANS involves treating symptoms with cognitive behavioral techniques, psychiatric medications, immunosuppressive therapies, and antibiotics. While these may all be necessary, they often do not provide long-term relief. An Integrative and Functional Medicine approach is essential in identifying and treating root causes and core clinical imbalances from which many of our children with PANS/PANDAS suffer in order to achieve long-term remission and put out the fire in their brains for good.
Dr. Song’s 6-Step Approach to PANS/PANDAS
Integrative and Functional Medicine recognizes that there is no one-size-fits-all approach, especially for a condition as complex as PANS/PANDAS.
Treatment must be individualized to your child’s unique story.
My 6-Step Approach to PANS/PANDAS is not a protocol. It is not an algorithm. It is a guide that incorporates conventional treatments with integrative and functional medicine strategies that must be tailored to each child. I am sharing it now in hopes that it may be useful for parents who are embarking on a PANS/PANDAS journey with their child, for children with PANS/PANDAS who are “stuck” in their treatment journey, and for practitioners who are on the front lines helping our children in need.
STEP 1: IDENTIFY & TREAT THE ROOT CAUSE(S)
Let history be your guide to know which tests are most appropriate to do initially. Remember that there may be infectious triggers (Strep, Herpes 6, Herpes 1 + 2, Coxsackievirus, Parvovirus B-19, Epstein-Barr virus, Influenza, Mycoplasma pneumonia, Lyme and other tick-born infections, etc), and non-infectious triggers (heavy metals, molds, and other environmental toxins). There may be multiple triggers. And new triggers may arise with each “flare.” Treatments must be targeted appropriately.
Steps should also be taken to support the immune system to reduce the frequency of acute illnesses which may cause your child to spiral into a PANS/PANDAS flare. Immune supports may include optimizing Vitamin D levels, ensuring a phytonutrient-rich diet that reduces inflammatory foods (gluten, dairy, sugar, pesticides, processed foods, etc.), and optimizing lifestyle (sleep, exercise, time in nature, stress management tools).
STEP 2: PUT OUT THE FIRE
Inflammation must be reduced to protect the brain. Pharmaceutical options include “conventional” treatments with steroids and NSAIDs. More natural options include omega-3 essential fatty acids, curcumin, and antioxidants such as vitamin c and glutathione. Anti-inflammatory diet and lifestyle as mentioned above are key in putting out the fire and keeping it out.
STEP 3: KEEP THE FIRE DOWN
“Conventional” PANS treatments suppress inflammation, but this inflammation typically returns as medications wear off or new inflammatory triggers arise. Inflammation in an acute setting of infections or toxins is NOT a bad thing – in fact, inflammation is required to fight infections or toxic exposures. But once inflammation has done its job, the immune system needs to send out signals that it’s time to settle back down and restore a healthy, normal immune response. Chronic, unchecked inflammation is the problem in autoimmune diseases like PANS/PANDAS.
What is needed is a way to modulate the immune response so that a healthy immune balance can be achieved and maintained. Other than IVIG, which is inaccessible to many and does not provide lasting results in others, there are no conventional ways to modulate the immune response. On the other hand, functional medicine offers a variety of options that I have found to be very helpful in restoring a healthy immune response to keep the fire down. These immunomodulatory treatments may include Low-dose naltrexone (LDN), Specialized Pro-Resolving Mediators (SPMs), CBD oil and Chinese Skullcap (Baikal or Scutellaria baicalensis).
STEP 4: ADDRESS CORE CLINICAL IMBALANCES
PANS/PANDAS treatments should not just be about “killing” the bug(s). The goal of PANS/PANDAS treatments should be about restoring the WHOLE CHILD back to a state of optimal health. A Functional Medicine approach that identifies and treats core clinical imbalances is essential for whole child healing.
These Functional Medicine interventions may include:
- Identifying and treating nutritional deficiencies and insufficiencies
- Optimizing the gut microbiome
- Treating a leaky gut and resulting food sensitivities
- Addressing mitochondrial dysfunction
- Optimizing methylation
- Supporting detoxification
STEP 5: RESTORE THE BODY-MIND-SPIRIT CONNECTION
PANS/PANDAS is a journey with many ups and downs. The psycho-emotional and socio-emotional toll that PANS/PANDAS takes on each child and family cannot be discounted. Supporting the emotional health of the child and family with cognitive behavioral therapy, counseling, and support groups for the child, siblings and parents is essential. Stress management, mindfulness tools and vagus nerve work to restore the parasympathetic “rest-digest-heal” state are essential to not just restoring the mind, but to maintaining healthy immune, gut, and nervous systems. Read more about why this is so important in my article 6 Steps to a Stress-Proof Child.
STEP 6: INTEGRATIVE CARE
Be open and explore “alternative” modalities of care. Not one single practitioner has all the answers. And not one single treatment modality offers all the tools that your child may need in their healing journey. Modalities that may be beneficial include Homeopathy, Essential Oils, Acupuncture, Chiropractic, Osteopathy, and Energy Medicine, to name a few.
You can download my FREE 6-Step Approach to PANS/PANDAS HERE:
My parting message to you
To the mama and papa heroes going through a PANS/PANDAS journey with your child:
- Don’t give up
- Keep looking for answers, the right practitioner(s), the right team …
- Don’t let anyone tell you that you, or your kid, is crazy
To the brave practitioners who are willing to believe, and to think outside the box…
- Thank you!
- We need more of you!
- (For practitioners who want to learn more about my integrative pediatric approach to PANS/PANDAS and other chronic pediatric conditions, review cases, and get more mentorship, training, and support in pediatric-specific functional medicine, I created my Healthy Kids Happy Kids Practitioner Membership for you. I’d love to support you and see you inside.)
We’re all in this together.
xo Elisa Song, MD
PANS/PANDAS Resources:
Dr. Song’s Talks:
- Fx Medicine podcast PANDAS Part 1
- Fx Medicine podcast PANDAS Part 2
- New Frontiers in Functional Medicine podcast on PANS/PANDAS Diagnosis & Treatment
Parent Online Resources
- Aspire
- The PANDAS Network
- New England PANS/PANDAS Network
- Northwest PANDAS/PANS Network
- Stanford Area PANS Parent Support Facebook Group – this group also has monthly calls with guest speakers often from the Stanford PANS Clinic
- The PANDAS Docs (Drs. Scott and Ellen Antoine)
- Institute for Functional Medicine Practitioner Database
Practitioner Resources
- PANDAS Physicians Network
- The Foundation for Children with Neuroimmune Disorders
- ASPIRE for Clinicians
- Medical Academy of Pediatric Special Needs (MEDMAPS)
- Institute for Functional Medicine
School Advocacy
- PANDAS and PANS in School Settings by Patricia Rice Doran
Books for Practitioners
- The Comprehensive Physicians’ Guide to the Management of PANS and PANDAS: An Evidence-Based Approach to Diagnosis, Testing, and Effective Treatment by Dr. Scott Antoine
- Demystifying PANS/PANDAS: A Functional Medicine Desktop Reference on Basal Ganglia Encephalitis by Dr. Nancy O’Hara
Books for Parents
- A Light in the Dark for PANDAS & PANS by Dr. Jill Crista
- Brain Under Attack: A Resource for Parents and Caregivers of Children with PANS, PANDAS and Autoimmune Encephalitis by Beth Lambert, Maria Rickert Hong, Roseann Capanna-Hodge, Jennifer Glustra-Kozek, Lauren Stone
- Childhood Interrupted: The Complete Guide to PANDAS and PANS by Beth Alison Maloney
Books for Kids
- In a Pickle Over PANDAS by Melanie S. Weiss
- What To Do When You Worry Too Much by Dawn Huebner, PhD
- Outsmarting Worry by Dawn Huebner, PhD
- What To Do When Your Brain Gets Stuck by Dawn Huebner, PhD
References:
- http://www.aappublications.org/news/2017/03/28/Pandas032817
- PANDAS Parent Survey April 2014, San Francisco
- Okano Motohiko, Matsumoto Shuzo, Osato Toyoro, Sakiyama Yukio, Thiele Geffrey M,. Purtilo David T. Clinical Microbiology Reviews, January 1991, 4(1): 129-135. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC358181/pdf/cmr00042-0145.pdf
- http://www.moleculeralabs.com/cunningham-panel-laboratory-testing/
- Thienemann Margo, Murphy Tanya, Leckman James, Shaw Richard, Williams Kyle, Kapphahn Cynthia, Frankovich Jennifer, Geller Daniel, Bernstein Gail, Chang Kiki, Elia Josephine, and Swedo Susan. Journal of Child and Adolescent Psychopharmacology. July 2017, ahead of print. https://doi.org/10.1089/cap.2016.0145
- Frankovich Jennifer, Swedo Susan, Murphy Tanya, Dale Russell C., Agalliu Dritan, Williams Kyle, Daines Michael, Hornig Mady, Chugani Harry, Sanger Terence, Muscal Eyal, Pasternack Mark, Cooperstock Michael, Gans Hayley, Zhang Yujuan, Cunningham Madeleine, Bernstein Gail, Bromberg Reuven, Willett Theresa, Brown Kayla, Farhadian Bahare, Chang Kiki, Geller Daniel, Hernandez Joseph, Sherr Janell, Shaw Richard, Latimer Elizabeth, Leckman James, Thienemann Margo, and PANS/PANDAS Consortium. Journal of Child and Adolescent Psychopharmacology. July 2017, ahead of print. https://doi.org/10.1089/cap.2016.0148
- Cooperstock Michael S., Swedo Susan E., Pasternack Mark S., Murphy Tanya K., and for the PANS PANDAS Consortium. Journal of Child and Adolescent Psychopharmacology. July 2017, ahead of print. https://doi.org/10.1089/cap.2016.0151
Thank you. I wish I would have understood about the difference between Pans and Pandas long ago. The only thing that I knew was that Strep was involved…no idea that that isn’t the only trigger. My oldest suffers from OCD. There was a sudden change around 4. I so wish I had known these things earlier.
My heart goes out to you. I hope your oldest receives the treatment needed for recovery. xo